Abstract
Introduction :
Thrombocytopenia is a common problem in hospitalized patients. One of the rare but fatal causes of thrombocytopenia is Heparin Induced Thrombocytopenia (HIT), a complex immune disorder in which heparin leads to the production of IgG antibodies, targeting platelet factor 4 (PF4). Not diagnosing HIT when it is present or mistakenly diagnosing HIT when it is absent, both carry significant risks (eg, life-threatening thrombosis or life-threatening bleeding, respectively). Various institutional reviews have reported that clinicians tend to have a high suspicion and low threshold to order laboratory workup for HIT though the incidence of HIT is noted to be only 5%. The American Society of Hematology Choosing Wisely Guidelines 2014 recommend against testing for HIT in individuals at low risk, defined by a 4T score ≤ 3.
The primary objective of our study was to examine compliance with guidelines at our institution. Secondary objectives were to assess correlation between 4T's score, HIT antibody and Serotonin Release Assay (SRA) in diagnosis of HIT, impact of Hematology consult on following appropriate guidelines.
Methods:
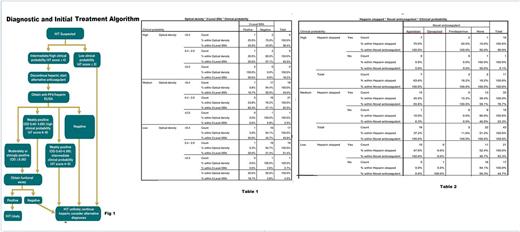
Patients with requests for HIT antibody testing between 1/1/2015 - 12/31/2016 were identified from laboratory records. A retrospective chart review was conducted on 92 patients who met criteria. Data collected included admitting department, clinical probability based on 4T's score, result of HIT antibody including optical density (OD), result of SRA, placement of Hematology consult, initiation of novel anticoagulant (NOAC). Using the algorithm below ( Fig 1) , compliance with guidelines was analyzed. Data were tabulated by means of simple frequencies for single items, or in 2- or 3-way combinations.
Results:
Of the 92 charts reviewed, 38 (41.3%) patients had a low clinical probability based on 4T's score and yet had HIT antibody test ordered (table 1). Of these, heparin was stopped in 21 (55.3%) patients and NOAC was initiated in 10 (26.3%) patients (table 2) which is not recommended as per existing guidelines. Interestingly, of the 38 patients with low probability, 19 (50.0%) had OD between 0.4 - 1.99 with 1 positive SRA. Among 43 (46.7%) patients with intermediate clinical probability, 29 (47.5%) patients were HIT positive. Of these, 18 patients with OD < 2 and 21 patients with OD between 0.4 - 1.99 had SRA ordered which is not in compliance with guidelines, however 6 of these patients had positive SRA. 11 (12%) of the 92 patients had high clinical probability, and of these, in patients with OD> 2, SRA was positive 100% of the times; where as in patients with OD between 0.4 - 1.99 SRA was positive only in 45.5% patients. Hematology oncology service was consulted for 44 (47.8%) patients with positive HIT of which 7 had high probability, 22 had intermediate probability and 15 had low clinical probability; heparin was stopped and NOAC was initiated in 5(71%), 12 (54%), and 8 (53%) patients in each of these groups respectively which once again is not in compliance with existing guidelines. Majority of patients were admitted to ICU, however only 3.8% of ICU patients who had HIT antibody ordered had confirmed diagnosis of HIT.
Conclusion:
Compliance with Choosing Wisely Guidelines and recommended diagnostic algorithm for HIT at our institution is low, and potentially associated with significant harm to the patient due to overtesting and overtreatment. Hematology Oncology consult did not necessarily improve compliance with guidelines, although decision about NOAC were made prior to consult in most cases. However, while there was concern for overdiagnosis and wasteful resources, our study also noted that there were few patients with low clinical probability and intermediate clinical probability with OD between 0.4-1.99 with positive SRA. Limitations of our study is the small sample size and single institution based data.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal